Type of publication:
Post on the Academy of Fab NHS Stuff website
Author(s):
*Lewis, Jules; *Lock, Jules
Full text:
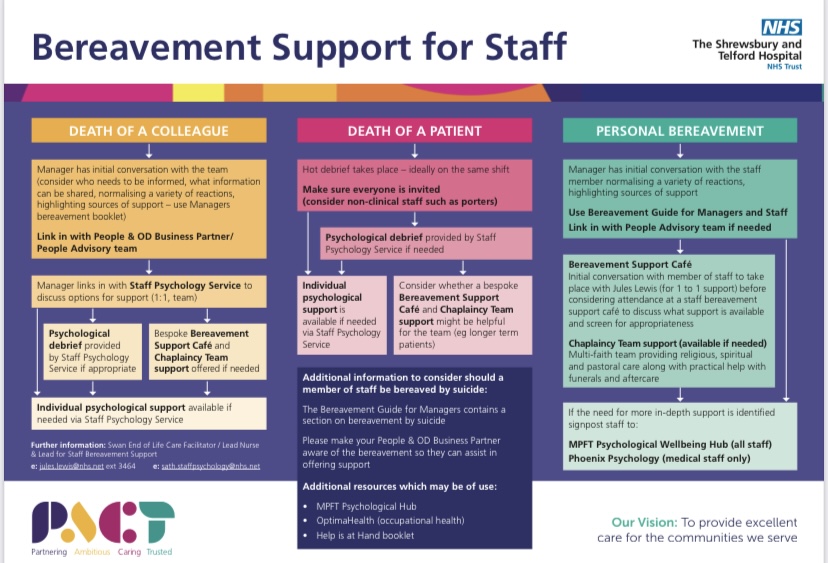
The OWEN Model (2022) has been created by the SWAN End of Life Care Lead Nurse Jules Lewis and SWAN Lead End of Life Care Volunteer Jules Lock. The service to deliver this staff bereavement intervention has been mapped out, please see attached poster for evidence.
O- Openness. Staff are given the time and space, to share their feelings about the death of a loved one or a patient they have cared for.
W- Wellbeing. The wellbeing of the staff is at the centre of the support we give. Signposting to other services is offered as appropriate. The needs of the staff will vary greatly.
E- Empathy. Compassion, kindness, understanding and support, are at the centre of the model. The use of appropriate and kind language is key to everything we do.
N- New Beginnings – Recognise that grief can remain with us for the rest of our lives. Enabling staff to move forward with hope, whilst never forgetting the person who has died. (SaTH 2022).
Bereavement and grief can impact all our lives at some time. The way we cope with grief and loss is unique and people will react in so many ways. There is no time scale to grief and support can be needed at many different times along that journey. Health care staff can be affected by personal grief and through their professional life. Staff who look after patients with long term conditions, will form friendships with those patients and the families. The loss of these patients can be very upsetting, and this should be factored into the care provided within a trust.

The OWEN Model offers one to one support and signposting as appropriate and ongoing peer support in the form of staff bereavement support cafes (as seen on BBC1 Extraordinary Portraits series 3 episode 4) & supported by The Good Grief Trust, help & hope in one place. Looking after our staff at the hardest of times, so they can look after others. This work is in memory of Joan Owen a kind, caring and much loved & missed lady. Thank you to Joan’s family for their support. Thank you to Penny Watson our SWAN End of Life Care Administrator who supports this work & Debbie Snooke and Miriam Gilbert both SWAN End of Life Care Specialist Nurses.


